

Conversely, airway resistance increases during forceful expiration due to flow-limiting segments. Īirway resistance is inversely proportional to lung volumes which means during inspiration, airway resistance decreases, especially in small bronchioles, to enhance expansion. as shown in Figure 1, changes in lung volumes in obstructive vs. So, patients with more compliant lungs shift the curve to the left, and higher volume can be achieved with low pressure. For stiff lungs (less compliance), the curve is shifted to the right, so lower volume is achieved for any transpulmonary pressure. So, diseases affecting the alveoli may disrupt compliance making the lung either stiffer (more resistant to expansion) or less stiff (easily expandable). That means the elastic tissue of the lungs at this point cannot be stretched further, and no additional volume of air can be added. So, the compliance relationship (pressure-volume relationship) between transpulmonary pressure and the volume inside the lungs can be represented by a curve that flattens at high distending pressure when the lungs reach their upper limit of expansion.
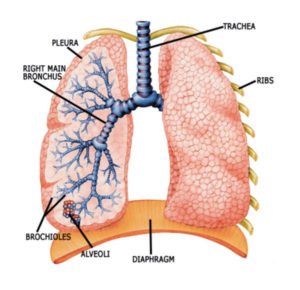
Thus, the difference between the positive pressure (from airways) exerted on alveoli, and negative pressure in the pleural space is called transpulmonary pressure. During inspiration, contraction of the diaphragm creates negative pressure around the lungs allowing the lungs to expand in addition to the positive pressure exerted on the lungs from the airways. Īnother important part of lung physiology is compliance which simply means the opposite of stiffness. CO 2 diffuses more readily than O 2 because of its high plasma solubility. The barrier to this process includes a cytoplasmic extension of type 1 cells, the basement membrane, and the capillary endothelial layer. This difference results in the diffusion of O 2 from the alveolus to the capillaries. Gas exchange between the alveolus and the blood capillary depends on the passive diffusion of PO 2 in the alveolus (around 100 mmHg), and the blood entering the capillary (around 40 mm).


 0 kommentar(er)
0 kommentar(er)
